MYOCARDIAL INFARCTION
Definition:
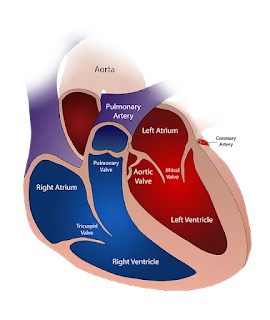
- Myocardial Infarction is defined as " a diseased condition which is caused by reduced blood flow to the coronary artery due to atherosclerosis and occlusion of artery by embolus or thrombus."
Myocardial Infarction (or Heart attack) is the irreversible damage of myocardial tissue due to prolonged ischemia or hypoxia.
Universally accepted definition of MI: Evidence of myocardial necrosis in consistent with the myocardial ischemia, in which case any of the following meets the diagnosis of Myocardial Infarction.
- Evidence rises and/or fall of cardiac biomarkers (preferably troponin).
- ECG changes indicative of new ischemia (new ST-T changes or new left bundle branch block)
- Development of pathological Q waves.
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality.
Etiology:
- Tobacco smoking
- Diabetes Mellitus
- Age
- Hypertension
- Obesity
- Gender
- Stress
- Drug abuse
- Alcohol consumption
- Family history of ischemic heart disease (IHD)
- Chronic Kidney Disease (CKD)
- Hyperhomocystenima
- Hyperlipoproteinemia
Etiopathogenesis:
- Acute plaque rupture
- Myocardial ischemia
- Non-atherosclerotic cause
- Transmural v/s subendocardial infarcts
- Role of platelets
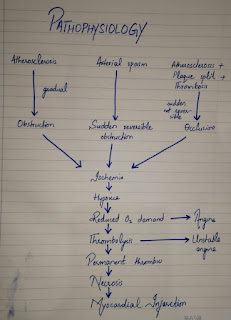
Pathophysiology
Clinical Presentation:
- Chest pain
- Dyspnea
- Fatigue
- Sweating
- Weakness
- Nausea
- Vomiting
- Light headache
- Palpitation
- Anxiety
- Sleeplessness
- Hypertension
- Hypotension
- Arrythmias
Complications:
- Arrythmias
- Cardiogenic shock
- Congestive Heart failure
- Thromboembolism
- Pericarditis
Diagnosis/Investigation:
- Clinical Features: Apprehension, Fever, Pain, Shock, Indigestion.
- Serum cardiac Markers:
- Creatinine phosphokinase (CK)
- Lactic dehydrogenase (LDH)
- Cardiac specific troponins (CTN)
3. ECG changes: ST segment elevation, T wave inversion, Appearance of wide deep Q wave.
4.Other Tests: MRI, Angiography, Position emission tomography (PET scan). Chest X-ray, Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein (CRP).
Management:
1.Non-Pharmacological Treatment:
- Counselling and education to patients.
- Alcohol consumption cessation.
- Smoking cessation
- Lifestyle measurement
- Diet and nutrition
- Salt Restriction
2.Pharmacological Treatment:
- Anti-Thrombolytic Therapy:
- Antiplatelets-to reduce the aggregation of platelets such as Aspirin, Clopidogrel, Ticagrelor.
- Anti-coagulants- that reduces the risk of thromboembolic complication and prevents reinfarction in the absence of reperfusion therapy.
2. Anti-hypertensive agents:
- Glyceryl trinitrate sublingual, IV nitrates
3. Lipid Lowering Agents:
- Reduction of cholesterol through diet and drugs helps reducing morbidity and mortality.
4. Vasodilators:
- Beta blockers
5. Others:
- such as Analgesics, IV Opiates (morphine sulphate or diamorphine 2.5-5mg), IV anti-emetics (initially metoclopramide 10mg), Anti-ulcers, Antidepressants
6. Reperfusion Therapy:
- Depending on the type of MI, outcome of reperfusion therapy varies:
NSTEMI (Non-demonstrable benefit)
STEMI (Restores coronary artery patency, improves ventricular function and improves survival)
7. Percutaneous Coronary Intervention (PCI)
8. Thrombolysis:
- It reduces hospital mortality by 20-50%.
- Alteplase (human tissue plasminogen activator). over 90 minutes (15mg bolus dose), followed by 0.75mg/kg bodyweight not exceeding 50mg over 30 minutes. Then 0.5mg/kg body weight, not exceeding 35mg over 60 minutes.
- This has better survival rate than other thrombolytics.

Comments
Post a Comment